Treating the Whole Patient: Why Is It Important and How Can It Be Done?
When a patient goes to their healthcare provider, they bring with them a complex and interconnected set of circumstances that contributes to the development and exacerbation of their conditions. While it’s very common for doctors to see the person sitting before them as a composite of symptoms, and a problem to be solved, there is usually much more at play that needs to be addressed during the care process.
Even though a person might present with heart disease, there is a host of co-occurring factors that can lead to the diagnosis, the worsening of the condition, and even the derailment of the treatment regimen. Whether it’s their emotional health, their family relationships, their living situation, or any other seemingly unrelated factor, these situations can take a serious toll on a person’s overall health and their quality of life.
The term “holistic” treatment is used to describe treatment of the totality of the condition and has become one of the healthcare landscape’s favorite buzzwords. Another term for the process is the “whole patient” treatment model.
Importance of Treating the Whole Patient
To better understand the critical importance of treating the whole patient, let’s first examine two key statistics:
The Centers for Disease Control and Prevention (CDC) reports that over 60 percent of Americans currently suffers from at least one type of chronic illness, and 40 percent suffers from more than one.
The agency also reports that eliminating three risk factors malign lifestyle obstacles, like poor diet, inactivity, and smoking – would prevent approximately 80 percent of heart disease and stroke; 80 percent of of Type 2 diabetes; and 40 percent of cancer.
Within the context of each of these lifestyle factors, and many others, there are virtually endless scenarios that can inflame episodic frequency and get in the way of behavioral changes that are key to success. In other words, what we do in the moment, however ill-advised, affects how we feel later; and life is comprised of a series of moments.
The whole-patient approach to healthcare goes beyond “How are you feeling?” to ask: “Why are you feeling that way?”, and on a more granular level, “What lifestyle circumstances are affecting your decision making and behavior to make you feel that way?”
Treating the whole patient also allows patients to feel more heard and respected, and it goes beyond the often-rigid care that doesn’t line up with patients’ individualized needs.
What’s Involved with Treating the Whole Patient?
On a practical level, effective implementation of the whole-patient treatment model depends on cooperation, between multiple types of care providers (GPs, psychologists, dieticians, cancer specialists, and even those outside of the medical landscape, like caseworkers and specialized program administrators). To maximize patient outcomes, cultivate long-term health-driven behavioral changes, and get patients to proactively prioritize their health, providers must meet patients where they are: functionally, emotionally, and socially. They must understand their patients’ values (and we’re not just talking about cholesterol, blood pressure, or BMI).
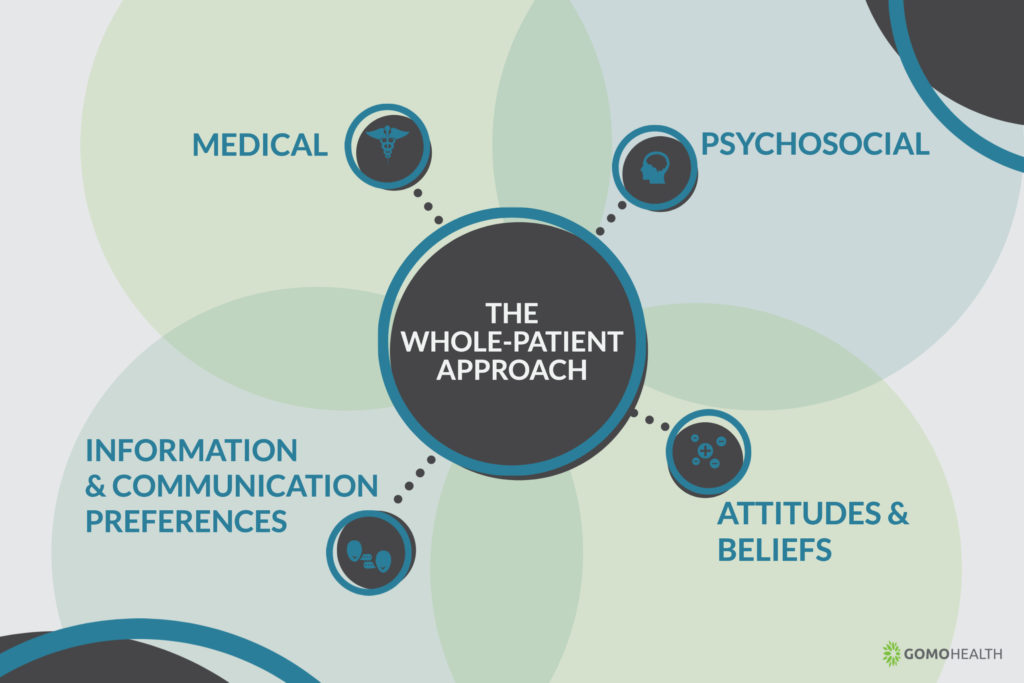
The Mayo Clinic has launched an entire initiative around the whole-patient approach, and breaks out the levels of care that patients will experience throughout their care cycle. The model is broken up into several distinct areas that encompass the patient’s care needs: medical, psychosocial, attitudes and beliefs, and information and communication preferences.
Medical – Being Patient with the Patient
If a patient is struggling with multiple health issues, they usually see their conditions as interconnected, and seeking treatment beyond compartmentalized symptom management. If a person suffers a heart attack, falls, hits their head, and develops neurological issues as a result of the impact, heart disease just became one of many problems on a list of many. Nonetheless, patients routinely report frustration that their doctors don’t see their conditions as related and fail to discuss holistic treatment options with them. An article in the Atlantic highlighted one woman’s 15-year quest for a diagnosis because her doctors and nurses were not hearing her during her visits.
Psychosocial – Where We Live Is How We Live
The Robert Wood Johnson Foundation, as well as other healthcare leaders report that things like the quality of our schools, affordability and stability our housing, access to good jobs with fair pay, and the safety of our neighborhoods can keep us healthy in the first place. The places we go, the people with whom we associate, and the values we cultivate as a result directly inform thing like nutrition, medication adherence, emotional health, and other areas integral to long-term wellness.
On a purely clinical level, psychosocial paradigms address the relationship between emotional and physical health issues, and how they affect one another; for instance, stress-related high blood pressure, anxiety-related Crohn’s disease, diagnosis-related depression, etc. A person’s emotional state throughout the care process will directly inform their daily and long-term choices, as well as their overall level of buy-in toward their ongoing care.
Attitudes, Beliefs and Value Systems
The Attitudes and Beliefs component of the whole-patient approach deals with the management and prioritization of one’s own care through their own experiences or those of a friend or family member. It may not sound like it makes much of a difference, but the reality is that one bad hospital experience, or even an unpleasant anecdote from a loved one, can come into play when making daily and long-term decisions about how often we go see doctors, and what it takes to get us to make an appointment. This cycle of behavior comprises the “Beliefs” component.
To maximize patient outcomes, cultivate long-term health-driven behavioral changes, and get patients to proactively prioritize their health, providers must meet patients where they are: functionally, emotionally, and socially.
Attitude includes general predisposal in one’s own care. This is often linked to experiences and beliefs, and providers can do their part to either nurture or alter these attitudes. If someone has very little interest in getting involved in their own, their doctor or care provider can work with them to improve their buy-in; if a patient is more engaged in learning about the treatment and management of their diagnosis, their doctor can nurture that attitude, and provide information.
Information and Communication Preferences
The most valuable information in the world can quickly become the least valuable if the transmitter fails to reach the receptor, which is why the Information and Communication Preferences component of the whole-patient model is critical. It deals with how patients learn, when patients are open to learning, how patients seek out information, and how they prefer to exchange information with a care team. More and more, AI and electronic communication are playing a key role in the Information and Communication Preferences component, because they allow for quick, logistically friendly and effective interaction with care providers, and exchange of valuable information.
GoMo Health understands the close relationship between information exchange and the whole-patient model, and we’ve emerged as innovators in the field of personalized patient engagement through electronic communication. We’ve helped healthcare organizations in practically every area of specialization more readily embrace the whole-patient model by making it easier to communicate with their patients and offer valuable, and often lifesaving, insights on their conditions.
As the focus toward patient care moves further and further toward a holistic model, connecting with patients through mobile technology is, and will continue to be, a key piece of the puzzle.
Treat the person, not their disease
Find out how GoMo Health is forming holistic care models with health systems, hospitals, and health plans







Find Us Online