5 Critical Facts about Adherence and their Implications for Population Health
Non-adherence for patients with chronic diseases such as diabetes or hypertension is extremely common – more common than you might think. Furthermore, non-adherence is largely perceived as a “patient issue” and not a massive problem with implications for physicians or health systems.
However, the results of non-adherence impact healthcare providers greatly, resulting in hospital readmissions, rising costs of care, and even higher rates of morbidity. In this new value-based world of health care, adherence is a crucial link between treatment and outcomes for a patient.
The critical facts surrounding non-adherence
1. Most of the top barriers to adherence are behavioral or cognitive in nature or are related to the patient’s environment. These top barriers include:
- Lack of motivation
- Depression
- Denial
- Cognitive Impairment
- Cultural issues
- Low educational level
- Alternate belief systems
- Complexity of treatment
- Side effects or fear of side effects
- Inconvenience
- Cost
- Time
2. Medication non-adherence results in an estimated 125,000 preventable deaths a year.
3. It’s been estimated that roughly half of the 3.2 billion medications prescribed in the U.S. every year aren’t filled or taken as prescribed.
4. Non-adherence worsens morbidity. Approximately 33% to 69% of medication-related hospital admissions are due to poor adherence.
5. Healthcare costs ranging from $100-$300 billion have been attributed to non-adherence in the U.S. annually. This comprises 3% to 10% of total U.S. health care costs.
Increase patient activation by adjusting behavior patterns
“Increasing the effectiveness of adherence interventions may have far greater impact on the health of the population than any improvement in specific medical treatments.”-World Health Organization
By improving the adherence to prescribed medications, we can positively influence many facets of healthcare, including overall population health, costs of care, and hospital readmission rates. It is not easy for humans to alter their behavior, even for minor behaviors such as taking a prescribed medication. Each individual patient has their own set of motivators, behaviors, educational background, and barriers that impact the activation (or lack thereof) of their care.
In order to increase medication adherence, it is important to treat the entire person, not just their condition. Through a combination of Behavioral Psychology and Cognitive Neuroscience, increased resiliency in patients can be achieved in order to better engage them in their daily life, at home, at work, and at play.
GoMo Health applies its BehavioralRx science to our solutions for medication adherence in order to increase overall human resiliency. As a result, better outcomes are reported, and overall treatment care plans are more successful.
Real life applications to support care plan adherence
Gaps in Care
A gap in care is defined as the discrepancy between recommended best practices and the care that is actually provided. The most common gaps in care are:
- Individuals missing age-based or seasonal screenings or vaccines.
- Patients not consulting with doctors about a prescribed medication.
- Individuals not adding a medication to meet evidence-based guidelines.
Client Example: Monroe Plan for Medical Care

GoMo Health worked with Monroe Plan for Medical Care to increase patient vaccination compliance and care coordination for the plan’s younger members. By using Care Communications, Monroe was able to increase adherence rates in all of its patient categories.
Learn more about how Monroe Plan for Medical Care sought to increase HPV vaccination compliance among its young, at-risk members in our latest case study.
Transitions in care
Transitions in care refer to the movement of patients between health care practitioners, settings, and home as their condition and care needs change. This can include being discharged from the hospital, transitioning to a skilled nursing facility, or transitioning from an outpatient setting to inpatient admission.
Ineffective care transition processes lead to adverse events and higher hospital readmission rates and costs. One study estimated that 80 percent of serious medical errors involve miscommunication during the transition between medical providers.
Client Example: The Heart House
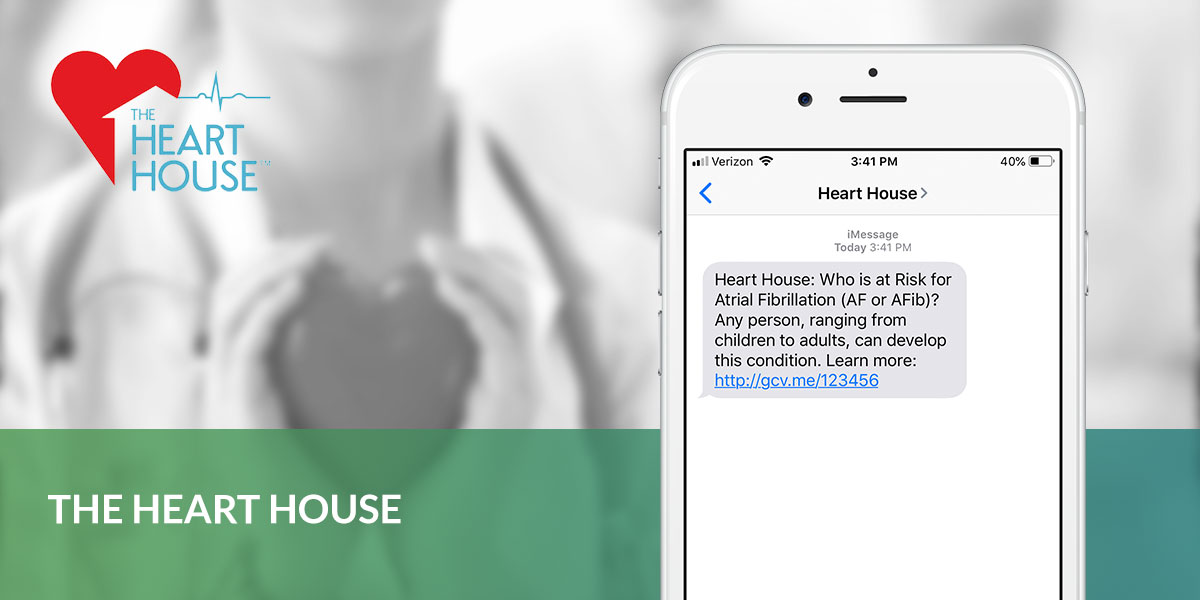
Patients at The Heart House are enrolled in a Personal Concierge program when they are either in treatment for a condition, discharged from the hospital, or are scheduled for a surgery. Care Communications are sent to them to guide them in important facets of their transition, including medication management, quality of life, device management, health literacy, and more. The program overall aims to improve patients’ condition, weight, wellbeing, and optimism about their future quality of life.
Quality of Life
Health-related quality of life is a multi-dimensional concept that includes facets of physical, mental, emotion, and social functioning. It focuses on the overall impact that health status has on quality of life and is related to well-being. Well-being assesses the positive aspects of a person’s life, such as positive emotions and life satisfaction.
Clinicians and public health officials use quality of life and well-being to measure the effects of chronic illness, treatments, and short- and long-term disabilities. Providing coping techniques, tips for managing side effects, and helping to change overall behaviors in people will positively influence quality of life and well-being for patients with chronic conditions such as asthma, diabetes, COPD, cancer, and more.
Client Example: Rutgers Cancer Institute of New Jersey
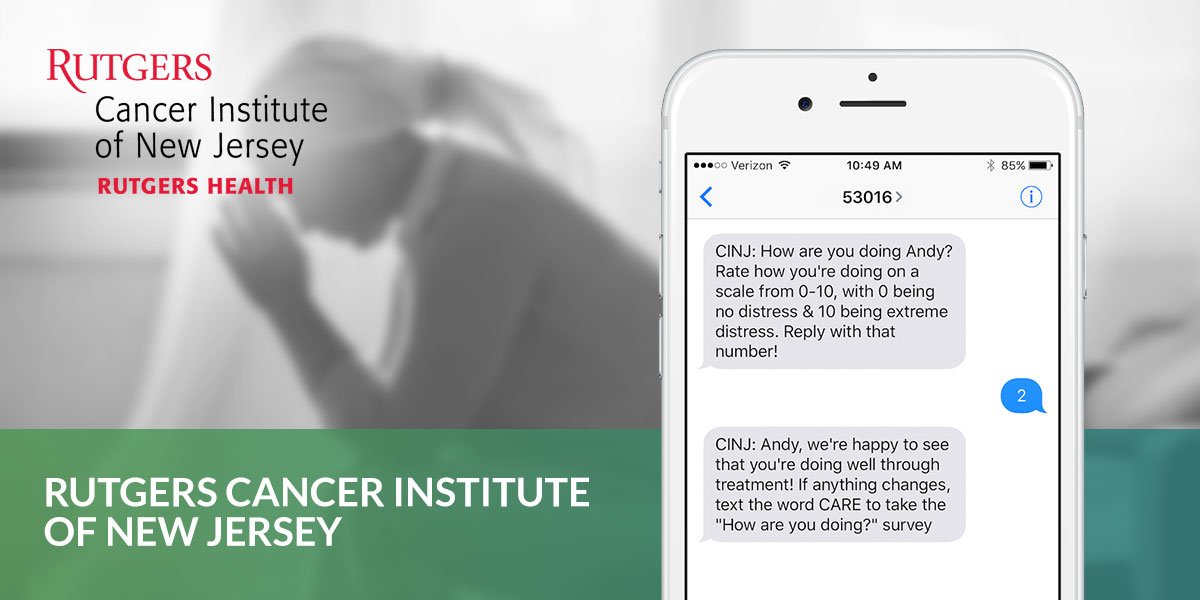
Rutgers Cancer Institute of New Jersey have implemented a program to ensure that their overall quality of life and well-being is supported for the lifestyle and care plans of cancer patients. This multi-faceted program seeks to address overall quality of life while ensuring that patients are meeting their care plan and seeking help if needed.







Find Us Online