The Future of Healthcare is in the Home
GoMo Health CEO and Chief Behavioral Technologist Bob Gold was featured in the Invest NJ 2022 North & Central Jersey report discussing the future of healthcare and the shift to at-home care models.
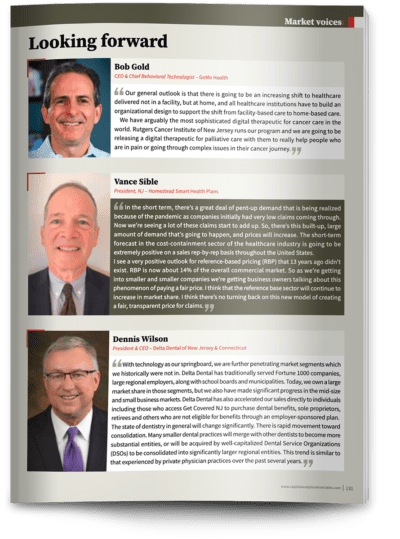
“Our general outlook is that there is going to be an increasing shift to healthcare not delivered in a facility, but at home, and all healthcare institutions have to build an infrastructure to support the shift from facility-based care to home-based care. We have arguably the most sophisticated digital therapeutic for cancer care in the world. Rutgers Cancer Institute of New Jersey runs our program and we are going to be releasing a digital therapeutic for palliative care with them to really help people who are in pain or going through complex issues in their cancer journey.”
Read on for a download on the future of at-home healthcare, including telehealth models, and the positive impacts of at-home care as evidenced by GoMo Health’s oncology digital therapeutic, a component of the Rutgers Cancer Institute of New Jersey remote care delivery model. The program has effectively improved the patient experience through targeted, personalized engagement, and in turn, has reduced the cost of care and adverse events within this population.
Demand for At-Home Care Accelerated Due to COVID-19 Pandemic
Strongly impacting increased worker shortages and filled-up hospital beds, COVID-19 completely transformed the healthcare industry, indicating a global need for new treatment methods. The Centers for Medicare and Medicaid have taken advantage of this opportunity, putting at-home care into action through the Acute Hospital Care at Home Program through which employees from 187 hospitals across 34 states are using digital therapeutics, mobile engagement, and video messaging to connect with patients.
Recent data demonstrates that, telehealth is being used 38 times more post-pandemic than pre-pandemic. Due to affordability, convenience, and accessibility associated with at-home care, this growing industry has received $29.1 billion in funding, becoming a primary go-to for treatment nationwide. Additionally, 40% of people expect telehealth to continue its growth and success.
How Can Providers Move from Facility-Based to Home-Based Care Delivery Models?
While there have been major improvements and advancements in at-home care delivery in recent years, providers must continue to cost-effectively shift clinical care delivery options into the home setting. There are many ways to activate this direction, including delivery of primary care services, outpatient-specialist consults, chronic disease management, hospice, and outpatient mental- and behavioral-health visits.
Acceleration of the at-home care model is also highly dependent on its economic viability and policies that address reimbursement. Currently, the payment model provides less incentive for healthcare organizations and provider groups to utilize and expand at-home care, which calls for new policies in payment innovation including value-based arrangements that could help incentivize these organizations.
Payers also play a large role in the adoption of at-home care as they can positively affect both providers’ and patients’ perspectives. In order to do this, payers could provide educational sessions and trainings to providers as well as look at at-home care coverage for patients to encourage utilization of these models.
Sophisticated Cancer Care Model at Work
While COVID-19 might have been a catalyst in exposing the opportunity to transition to at-home care and propelling the trend forward, GoMo Health has long-activated this patient-centered model through the delivery of digital therapeutics across many clinical areas, including oncology, as referenced in the Invest NJ feature. Cancer centers face ongoing challenges in ensuring optimal care coordination for cancer patients. By including digital therapeutics as part of an integrated care delivery model,, providers can respond to patient-reported stress/distress, monitor oral oncolytic medication adherence, identify warning signs of adverse events, and foster self-confidence for patients and caregivers.
The Rutgers Cancer Center Institute of New Jersey program is utilized to provide in-the-moment, personalized guidance and resources for patients with the inclusion of bi-directional surveys to screen patients regularly for signs of stress/distress, triaging responses with appropriate support and follow up, and escalating to the clinical care team as needed. In just under two years with 555 surveys completed, the GoMo Health automated bot was able to resolve 255 patient issues. Another 300 were escalated to the clinical care team for further support, in turn, reducing adverse events within this patient population.
Fill out the form below to download the full Cancer Institute of New Jersey Program results.







Find Us Online