A maternal population risk study
Mary E. Cramer PhD, RN, FAAN
Elizabeth K. Mollard PhD, APRN‐NP
Amy L. Ford DNP, RN
Kevin A. Kupzyk PhD
Fernando A. Wilson PhD
In Nebraska, nearly half of the counties on average – mostly rural – have a higher percentage of preterm births than the March of Dimes national average of 8.1%. Many of these rural counties are home to 30% or more soon-to-be mothers who receive inadequate prenatal care. Access to prevention and resources are rural barriers in Nebraska that contribute to preterm births.
Through a pilot study conducted under the direction of the University of Nebraska Medical Center (UNMC) and with funding from Blue Cross Blue Shield of Nebraska, we sought to positively impact these issues within Nebraska’s prenatal patient population. GoMo Health collaborated with Dr. Amy Ford and Dr. Mary Cramer from UNMC to develop a program with specialized content to help reduce preterm births.
Fill out the form to the right to download the study in its entirety.
Abstract
Objectives: (1) Assess feasibility of a smartphone platform intervention combined with Community Health Worker (CHW) reinforcement in rural pregnant women; (2) Obtain data on the promise of the intervention on birth outcomes, patient activation, and medical care adherence; and (3) Explore financial implications of the intervention using return on investment (ROI).
Sample: A total of 98 rural pregnant women were enrolled and assigned to intervention or control groups in this two‐group experimental design.
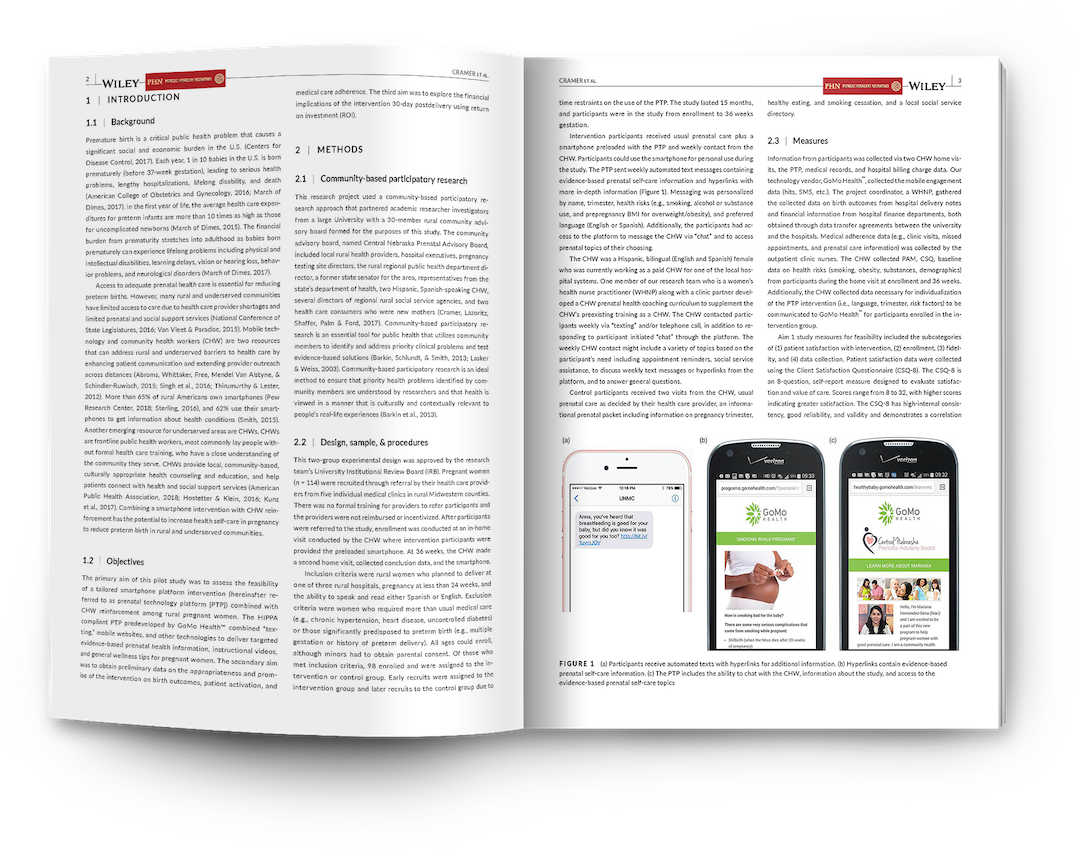
Intervention: The intervention group received usual prenatal care plus a smartphone preloaded with a tailored prenatal platform with automated texting, chat function, and hyperlinks and weekly contact from the CHW. The control group received usual prenatal care and printed educational materials.
Measurements: Demographics, health risk data, interaction with platform, medical records, hospital billing charges, Client Satisfaction Questionnaire‐8, satisfaction comments, and the Patient Activation Measure.
Results: A total of 77 women completed the study. The intervention was well‐received, showed promise for improving birth outcomes, patient activation, and medical care adherence. Financial analysis showed a positive ROI under two scenarios.
Conclusions: Despite several practical issues, the study appears feasible. The intervention shows promise for extending prenatal care and improving birth outcomes in rural communities. Further research is needed with a larger and more at‐risk population to appreciate the impact of the intervention.
Originally published in Public Health Nursing on September 14, 2018.



Find Us Online