High-Quality Healthcare for High-Risk New York Medicaid Members
Fidelis Care provides quality, affordable health insurance coverage for more than 2.4 million children and adults at all stages of life.
As a Medicaid program offering care management to high-risk members, the Fidelis Care Concierge provides a more personalized member experience and relevant education on conditions management while increasing the impact of the care plan by integrating the Personal Concierge program into day-to-day workflows.
| CLIENT OVERVIEW | |
|---|---|
| Website | https://www.fideliscare.org/ |
| GoMo Health Solutions | Personal Concierge™ GoMo Chat™ |
Our Goals
For Members:
For Case Management Team:

GoMo Health leveraged its proprietary emerging science, BehavioralRx, the science of precision health, to build the program and determine the engagement strategy, approach and content delivered.
The following behavioral and cognitive techniques were applied:
Personalized, Condition-Specific Education
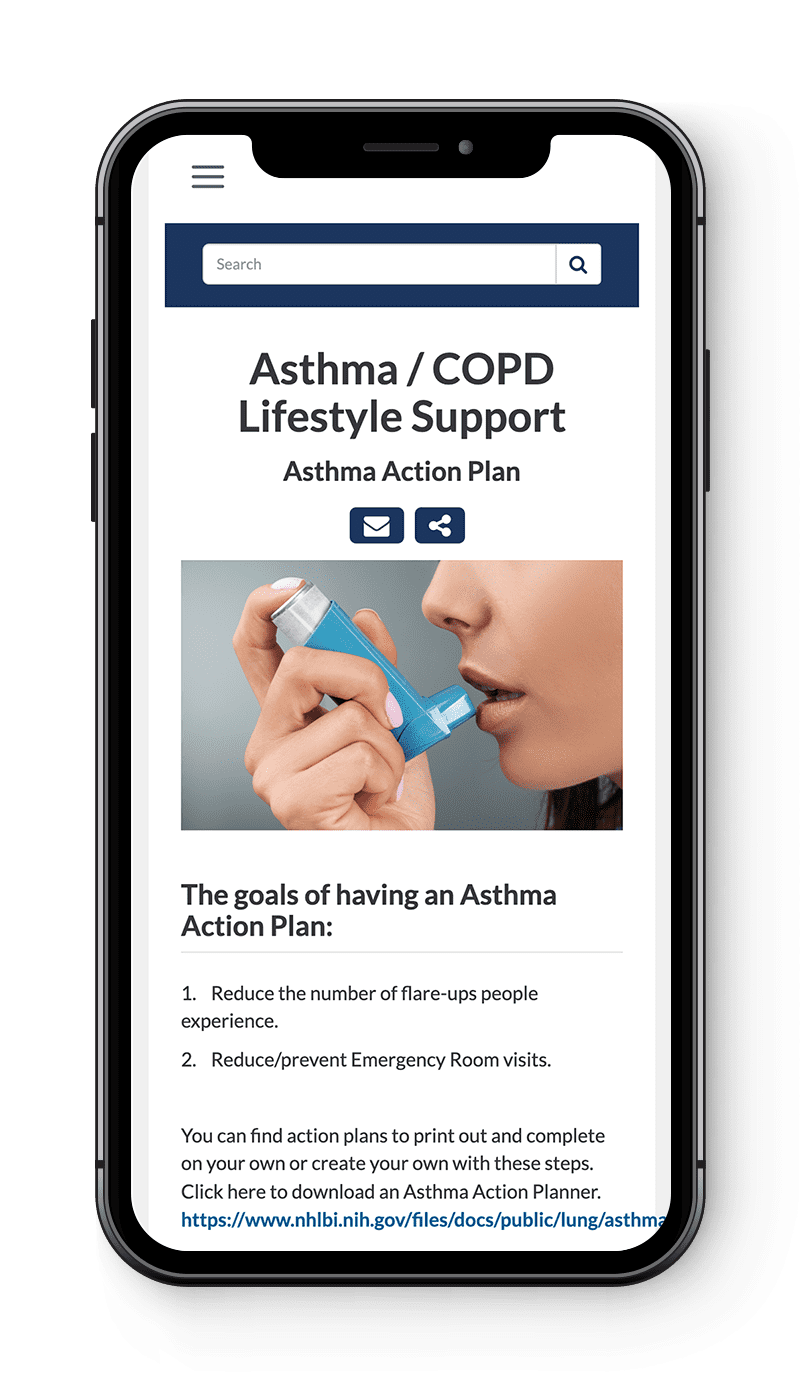
The concierge program serves members with chronic conditions who need advanced health management and care coordination by utilizing strategic health reminders and simplified access to local health, social and transportation resources, as well as live 24/7 help and triage options. Condition-specific content is delivered directly to each member’s mobile phone based on each participants’ content preference.
Qualifying conditions:
- Asthma
- Behavioral Health Management
- Congestive Heart Failure (CHF)
- COPD
- Diabetes
- High-Risk Pregnancies
- Medically Fragile Children
- Prenatal Women (with Substance/Opioid Use Disorders)
- Substance/Opioid Use Disorder
This program addresses each member’s self-expressed needs, social determinants of health and challenges, resulting in a more proactive approach to condition management and adherence to treatment. By leveraging this “tailoring technology”, participants are encouraged to submit ongoing candid feedback on their progress, enabling the program to be further customized to their individual needs.
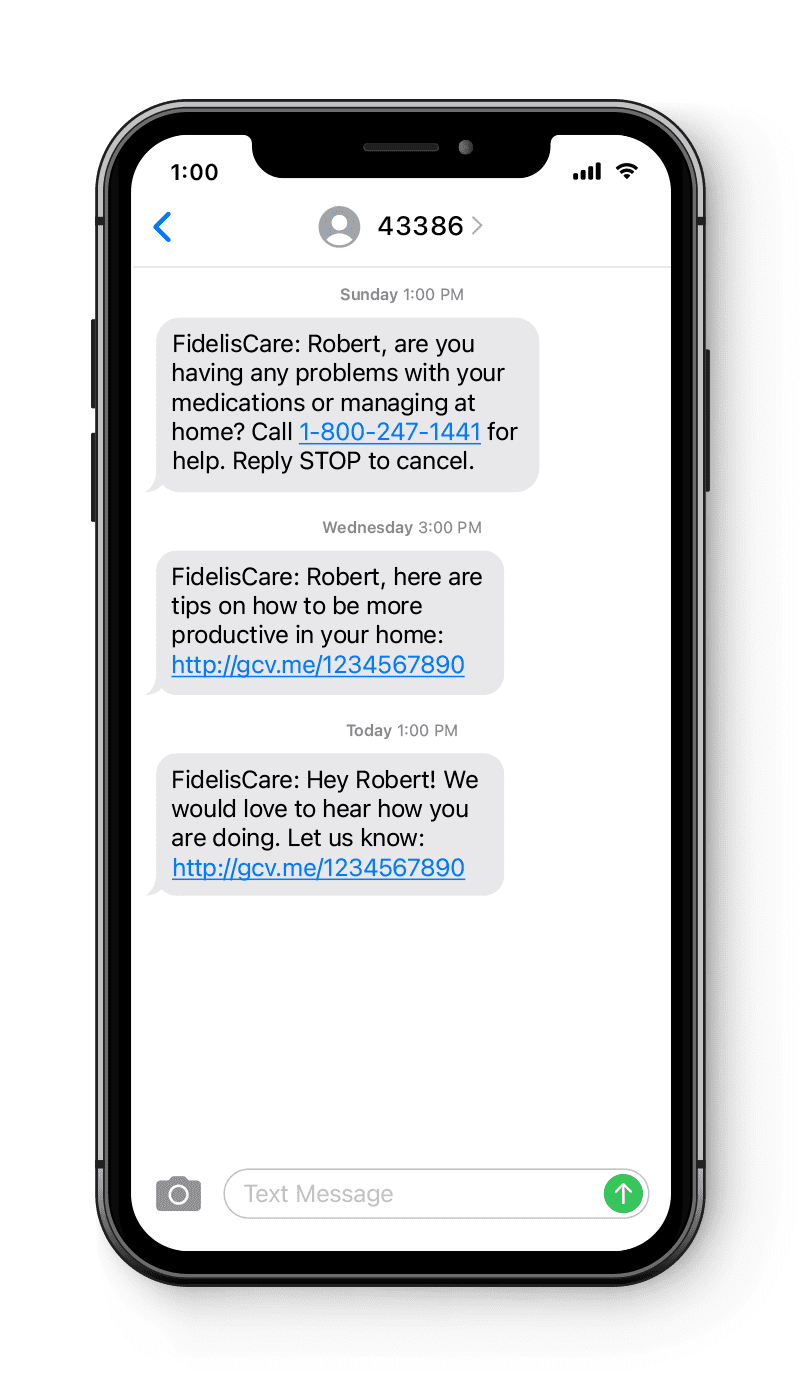
Meeting People Where They Are with Expanded Engagement
Members are prompted to complete surveys and feedback assessments, allowing the case management team to provide in-the-moment support for members. The program utilizes the GoMo Chat platform to connect with members one-on-one once feedback is escalated. This allows for the care management team to deliver highly personalized support in a streamlined way that saves time and resources and ultimately, reduces adverse events.
Program results:
- 6-7% closure in gaps in care for engaged members in multiple categories
- 4% reduction in ED visits
- 206% increase in case manager efficiency due to improved workflows that minimized staff burnout (measured by caseload per manager)
- 95% program retention rate






Find Us Online