The Heart of the Matter: Identifying and Addressing the Leading Causes of Hospital Readmissions for Cardiovascular Patients
The United States continues to see high rates of hospital readmissions for cardiovascular disease, despite the entirely preventable nature of these incidents. Data indicates that the national average for cardiac readmissions remains consistently at 21.9 percent.
Between inconsistent engagement with their healthcare providers, lack of adherence to diet, fitness regimen and medication routine, and a variety of other factors, many cardiac patients wind up back in the hospital, oftentimes with more urgent conditions than the first time they were admitted. One study from the University of Minnesota indicates that roughly 1 in 3 CVD hospitalizations resulted in 30‐day readmission; nearly 1 in 20 was followed by death within 30 days.
Even with more intuitive strides in telehealth services and patient education, congestive heart failure has been the leading cause of hospital readmissions throughout the country, ahead of septicemia and pneumonia. In an effort for care providers to effectively reduce these readmissions, it’s important to understand the most common causes. This requires examining both the clinical and behavioral journeys of patients living with heart disease. Let’s examine some of the causes of cardiac hospital readmissions.
Non-Compliance and Disengagement with Care Provider
Disengagement refers to a patient’s disinterest or lack of will to be active agents of their own care. Non-compliance means the unwillingness to stick to the core tenets of their care plan, particularly keeping their regularly scheduled follow-up appointments and completing other necessary tasks to make themselves healthier and minimize risk of a repeat event. Data from the University of Arkansas indicates that nearly half of all hospital readmissions patients don’t see their doctor for follow-up appointments. Although a certain level of obstinance and discomfort may play a role in this behavior, it’s usually because patients aren’t fully educated as to the importance of these treatment interventions and the risks that can arise when not followed.
Lack of Coherent Discharge Communication
When a patient leaves the hospital, especially for a cardiovascular condition, it’s critical that they get full and complete discharge communications including a list of instructions and insights to effectively manage their care at home. It’s also important that they continue to have access to their care provider to ask questions and prepare for any medical emergencies. Unfortunately, however, this is not always the case. Between poor discharge planning and issues following post-care instructions, interrupted transition of care following discharge continues to be an issue that leads to further incidents.
The Center for Medicare Advocacy reports that three of the main causes of hospital readmissions include premature discharge, lack of communication about disease management with patients and poor coordination with outpatient medical professionals who give care post-discharge.
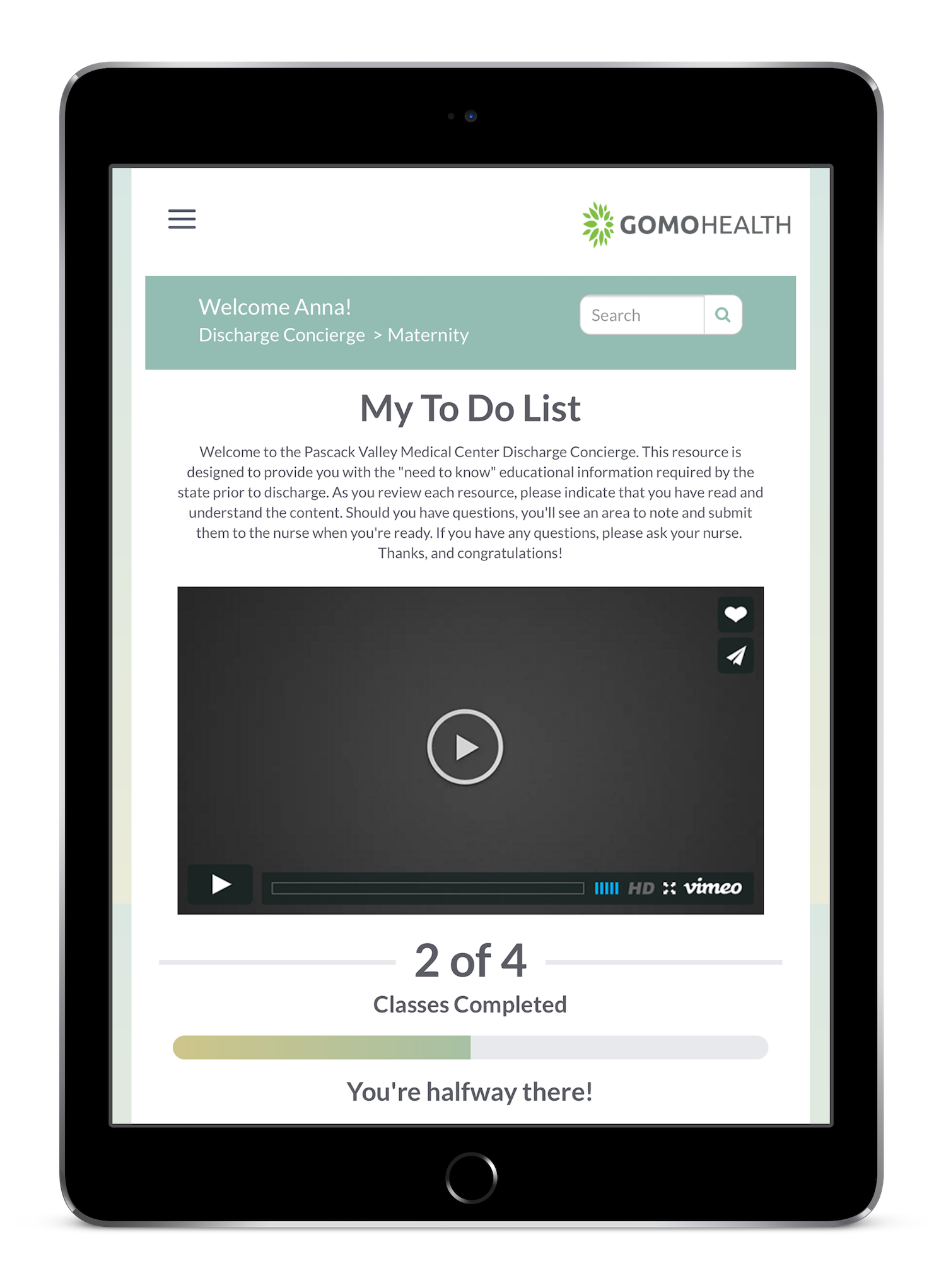
GoMo Health Discharge Concierge™ provides self-activated access to mandated information, allowing patients to read, understand, and acknowledge their comprehension prior to discharge. Learn more »
Post-Treatment Behavioral and Lifestyle Factors
It’s the hope of all care providers, to say nothing of loved ones of heart patients, that they follow their physicians instructions when it comes to nutrition, fitness and stress-reduction factors following their care, but that’s not always the case. Inability or lack of inclination to change lifestyle habits after cardiac care commonly lead to events resulting in readmissions. One recent study published in American Health and Drug Benefits revealed that measures like nutrition screenings and assessments saved local hospital systems nearly $5 million by reducing readmissions and shortening inpatient stays. Giving patients the educational, research-based and motivational tools, they need to maintain an active and healthy lifestyle after their treatment can considerably reduce their risk of an adverse event.
Coping with These Important Issues
When we examine the root causes of the primary reasons for hospital readmissions for cardiac patients, it’s easy to draw a direct line to lack of patient-provider engagement following discharge for their initial hospitalization. By engaging with patients in their lived environments, when they’re out of the doctor’s office and hospital room, providers can offer invaluable and consistent support for all areas of post-operative care, including medication adherence, nutrition fitness, and emotional support needs.
VIEW PROVEN RESULTS WITH OUR LATEST WHITE PAPER AND LEARN MORE ABOUT CARDIAC IMPLEMENTATION OF PERSONAL CONCIERGE™
Download our white paper created in collaboration with The Heart House, detailing their Cardiac Concierge Care Program. Learn how the program measured a 98% medication adherence rate (versus 40-50% for the national average) and a 43% decrease in tobacco use following program enrollment.






Find Us Online